#LettersHack: Is there a doctor in the room?
3 minute read
Our #LettersHack event in Leeds was an opportunity to get together and consider ways we might make primary care patient correspondence more user-centred and inclusive.
This month, we ran Letters Hack: Rethinking patient correspondence. Inspired by a similar event Citizens Advice held for energy customers and some great work done by Joe Bramhall and Kirsty Joan Sinclair, we've been planning the event for a couple of years.
This wasn't supposed to be the kind of hack where we throw pizza and beer at people and ask them to build something overnight, for free, that nobody really wants. We didn't ask but I don't think there were any coders in the room. Instead, the concept was intended to be a lo-fi, honest, unpicking of where stuff goes a bit wonky in health communications. From appointment booking, prescription ordering and use of GP websites, through interaction with online consultation platforms, to where patients find themselves in the primary to secondary care referral process. Research by the University of Bristol has shown that a shift to online can be a positive in some ways but also carries risks of excluding patients who struggle online, and inefficient systems create yet more work for practice staff who have to chase up incomplete information.
We looked at usability, accessibility (or lack of), talked openly about GP practice workloads and explored vendor responsibilities and the role of procurement. It felt practical. It also felt a little awkward, knowing the pressures on some of the people in the room and feeling a real need to avoid “design theatre" and condescension. Disclaimer: Post-Its were used in the making of this co-production. We had GPs, platform vendors, academics, people working in digital, user researchers, content and service designers in the room, all seeking to learn more. The structure of the day was (loosely) learn, listen, look more closely.

Learning
Lisa Drake, Redmoor Health
Lisa gave us a General Practice perspective on the spectrum of patient comms, including letters, SMS, texts, data, messages in applications, online forms and consultation platforms, websites and social media campaigns. As Lisa pointed out, it’s important to acknowledge that most people aren’t getting patient communications wrong on purpose. Instead, factors like a lack of staff training and turnover rates, asynchronous channels of communication and poorly designed online tools can all impact how comms are shaped and delivered. Lisa offered real-work examples of where stuff fails, for example SMS credit-based models that mean it’s more affordable to trim the parts of a text message that might just be the bit the patient relies on for trust and security.
Emma Parnell, Design for Joy
Emma talked to us about her time working in the NHS Digital team building the end-to-end national booking service for COVID-19 vaccinations. She told the story of a two-week period during the design and build phase where she pushed to ensure the service would be inclusive for people of any sex or gender. Emma gave us some background on the initial problem – two weeks before the service went live, the team discovered that to book an appointment, users would have to submit their gender to verify their identity against the personal demographic service (PDS) used for GP records. This would have the effect of excluding some people from the trans and non-binary communities.
The solution required work from technical architects, developers and content designers, along with testing with the trans and non-binary communities and consultation with NHS England’s LGBT Health Team. Eventually, Emma’s team were able to build momentum around the issue with the PDS eventually removing gender from the API as a mandatory field, and the gender question removed from the vaccine booking service altogether three months later. Emma’s story is a great example of how outdated infrastructure can create barriers to access for patients, and some of the complexities that come with unpicking such systems.
Sara Wilcox, Senior Content Designer, NHS Digital
As a Senior Content Designer for the NHS digital service manual team who coordinates work on the NHS style guide, we were delighted Sara joined us. Sara spoke to us about making health content easier to understand and how the service manual can help. This included some examples of misleading letters where overly complicated content and poor structure made information more difficult to understand.
Sara also talked us through the six principles behind the content guide itself and showed us the A to Z of NHS health writing which can offer a good basis for creating health comms in a clear and accessible way. This includes the importance of language. Using the examples of “pee" and “poo" (to great effect), we saw how less formal terminology may often be more understandable and accessible than formal terminology like “urine" and “faeces", which may confuse some readers.
These examples show the importance of considering the age, average literacy and numeracy level of the person reading your content. Sara showed us how the NHS Digital team had started from scratch to redesign their content by reducing reading time, making it easier to pick out and recall information, and introducing simpler navigation and clearer calls to action. Finally, and most importantly, the team tested their content on real patients, families and carers.

Listening
The conversations in the room highlighted the tension:
“We can't expect GPs to do usability testing"
“As clinicians, are you surprised some of the tech is inaccessible - NO".
“If they are winning contracts but saying their tech is compliant, they should be called out".....
We know from our own work that user research is embedded in the NHS Digital service guidance, and we are familiar with app library models, such as the ORCHA digital health review model, yet we are still seeing and hearing about usability and accessibility issues, platform workarounds, slow performance and poor integration.
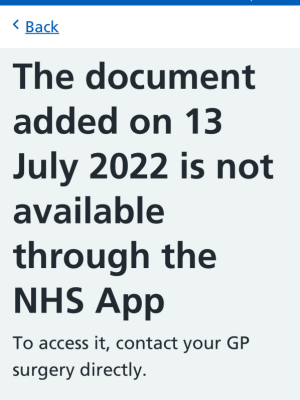
![NHS app, text reads "Automatic reply:Full access to my NHS records via the NHS app. We acknowledge receipt of your email, this email account is actioned Monday to Friday (NOT AT THE WEEKEND) between 9:00 am and 13:00 pm, anything sent after 13:00 pm will be looked at the following working day. For anything urgent please ring reception on [redacted]." The second half says slightly aggressively that medical symptoms must not be conveyed via email but rang into reception.](/media/5wxperpg/my-project-1-64.png?anchor=center&mode=crop&quality=80&width=300&upscale=false&rnd=133110776364530000)
Looking more closely
As a team at Nexer, we are lucky to help clients like Health Innovation Manchester, NeuroResponse, Bupa and NHS Digital work out approaches to engaging patients and clinicians in digital health. I have deliberately name-dropped those clients as they hint towards the complexity of “Healthcare". From discovery research, human factors, co-design, prototype testing, accessibility audits, and user research on care records, virtual wards and online consultations, we have covered a few perspectives. #LettersHack was intended to look at what works, what breaks, and when all of it gets communicated. We paused the event until we felt we could be in a room, with paper, scissors redacted letters, SMS printouts, A3 sheets showing long scrolling websites, passive-aggressive posters and aggressive-aggressive emails. All of it shows the strain on the system and the humans working in it.
A few years ago, we helped organise HomelessHack in Manchester. After a morning of talks, one of the team members put his hands up and said “honestly, as a developer, what can I possibly do to come up with anything this in a day?". This made us mindful of the perils of hackathons, where design saviours swoop like seagulls and crap on existing service delivery to invent a new portal or dashboard.
Our outcomes were more pragmatic and experimental and although the real value was in making connections and raising awareness, we did arrive at some practical steps for change:
- A place to share good examples, so we can build up some practical patterns. Inspired but the work led by Sarah Drummond on Mental Health Service Patterns, we are building a library of templates, resources and guidelines in Airtable
- To showcase each other’s work. Here we share the NHS content style guide and NHS Health A to Z guide and Iatro's library of resources for General Practice websites
- A commitment to ongoing sharing, now we’ve all met, again with a focus on what worked well, and reporting back on small experiments trialled
- A desire to mount collective pressure on what gets bought and built, raising the need for inclusive usability testing pre-procurement
It was a good day. The atmosphere was open, pragmatic and good-humoured, recognising the complexities and challenges everyone is facing, with a recognition that focusing on the small stuff might just take some things forward.
Thanks to all involved.

Get in touch
Please email hilary.stephenson@nexergroup.com if you would like to work with our team on your project, or call our Macclesfield office on +44 (0)1625 427718

